A Geisel-Thayer team at Dartmouth is investigating the individual and structural factors that promote resilience and allow medical students to flourish with the hope of finding ways to make medical school a less stressful experience.
It is well-documented that medical school is a high-stress experience with increasing rates of depression and anxiety among medical students who share an elevated risk of stress-related burnout with physicians and other healthcare professionals.
This escalating problem presents difficulties in attracting and retaining a healthy, flourishing medical workforce that can model wellness for their patients.
Using a biopsychosocial model for wellbeing to gather data in the wild, the interdisciplinary research team from the Geisel School of Medicine’s Departments of Medical Education, Biomedical Data Science, and Psychiatry, and Thayer School of Engineering are looking at data from wearable Fitbit devices and weekly app-based questionnaires to track well-being and resilience.
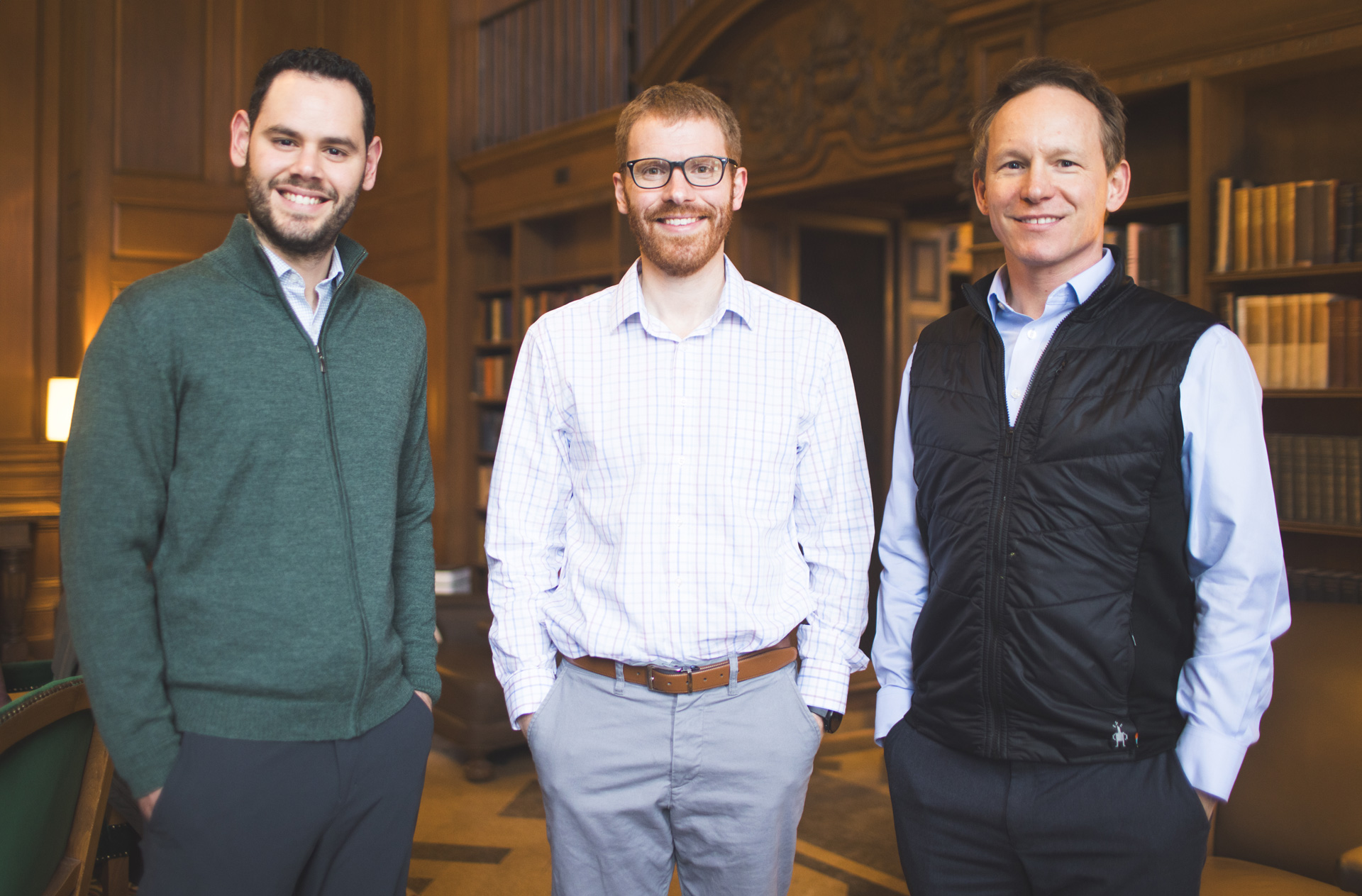
“Rather than focusing exclusively on ill health or mental illness, we also look at flourishing, the positive side of mental health that is so important to learning and living a fulfilling life,” says Thomas Thesen, PhD, an associate professor of medical education at Geisel and one of the principal investigators of the study.
Their research resulted in a Wearable Wellness Study. Launched in the 2023 academic year with medical students at Geisel, the study harnesses existing wearable technology to map physical activity, sleep, and heart-rate variability, all behavioral and physiological markers related to mental health, to understand individual and curricular factors that lead to not only high levels of stress, but also resilience. Thesen says the team hopes that insights from the study will lead to both more individualized support and curricular change to drive better student well-being.
First- and second-year Geisel medical students participating in the yearlong study each continuously wear a fitness tracker measuring heart rate, sleep, and physical activity that syncs with their smartphone. A smartphone app initiates wearable data collection and delivers weekly brief questionnaires, automated notifications, and reminders.
“Initiating this pilot study represents an important step in the ability to understand and reduce stress among medical students. We have consistently found that smartphone and wearable sensors can help in understanding and predicting mental health, and this effort expands our horizons,” says Co-Principal Investigator Nicholas Jacobson, PhD, assistant professor of biomedical data science and psychiatry in the Center for Technology and Behavioral Health at Geisel. “This study represents a demonstration of the profound potential of technology to cultivate a future where medical professionals can achieve optimal health and resilience.”
"Machine learning algorithms are a promising approach in predicting and addressing mental health conditions before they develop," says Co-Principal Investigator Wesley Marrero, PhD, an assistant professor of engineering at Thayer.
“Predictive models can assist mental health professionals in identifying medical students at increased risk for anxiety, depression, and burnout early in their education,” he says. “Moreover, they can serve as the foundation for algorithms focused on mental health interventions.”
“By collecting data across the curriculum, we can predict changes in well-being via machine learning algorithms. We are also looking at that in an aggregate way across all students to see which factors cause increased stress to help us make structural curricular changes,” Thesen notes.
Marrero is also interested in how to make sure there is equity across all people. "How do we make sure that we bring everyone up, and not just a majority population? That's called algorithmic fairness—accounting for people's intersectionalities and identities when making predictions and recommending interventions. That is a hard math problem, but one that's very interesting to work on."
Students participating in the wearable wellness pilot also have access to a companion program where they can elect to receive coaching to create a lifestyle management plan with goals monitored by their wearable device. If goals aren’t met, students and a coach work together to identify roadblocks and explore alternative methods to achieve their goals.
Because the study is collecting personal data about students, there is high level of data privacy protection in place—all collected information is anonymized, and identities are invisible, Thesen explains. The study employs a data monitor, a member of the medical school’s student government and who has veto power over any handling or analyses of the data that may be against the student’s interest.
This spring the study will be expanded beyond Geisel to include diverse student populations at two other medical schools—the University of Houston College of Medicine, a new medical school with a high percentage of students traditionally underrepresented in medicine, and the Medical College at Aga Khan University in Nairobi, Kenya.
Funding for both the initial pilot and the expansion of the study is provided by the American Medical Association through their ChangeMedEd and Precision Medical Education initiative.