When he began working at the NIH in 2016, Faraz Farhadi ’24, a fourth-year medical student at Geisel School of Medicine, could not predict how pivotal that experience would be to his career.
A research fellow in nuclear medicine and radiology in the Department of Radiology and Imaging Sciences at the institute’s Clinical Center, Farhadi became an assistant investigator for multiple clinical trials—work that produced more than 20 peer reviewed publications. And one patent.
Recruited in 2017 to a clinical trial to validate a prototype of the first-ever photon-counting CT scanner (PCCT) designed to improve quantitative image quality for low dose imaging, Farhadi and his colleagues investigated its application, utility, and safety profiling.

Farhadi worked with scientific and clinical investigators, including Babak Saboury, a radiologist and nuclear medicine physician, and Pooyan Sahbaee, a senior scientist from Siemens Healthineers, to design and conduct translational human and phantom studies on the technology. Their aim was to create clinical evidence covering aspects such as diagnostic accuracy, patient safety, and consistency in diagnostic spectral imaging, efforts that in 2021 contributed to the 510-K, FDA approval of the first clinical photon counting CT scanner—NAEOTOM ALPHA.
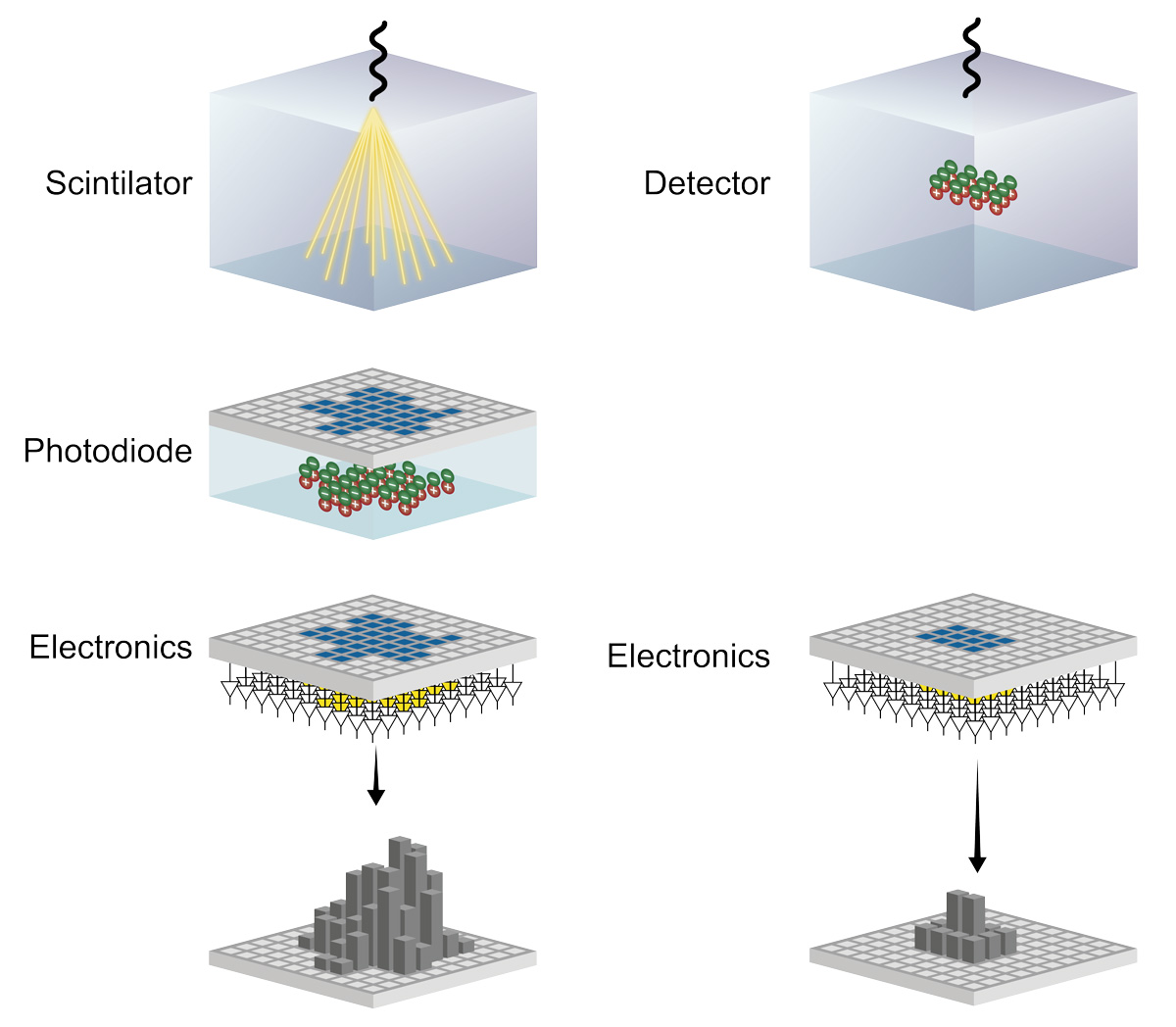
A computed tomography scan, developed in the 1970s and commonly known as a CT scan, is a versatile imaging technique used to capture detailed internal images of the body for medical diagnosis. CT scanners, Farhadi says, use energy-integrating detectors that measure the total energy contained in many X-ray photons during a measurement interval to create an electric signal. These cumulative electric signals taken from different angles are then processed on a computer using tomographic reconstruction algorithms to produce tomographic (cross-sectional) images.
“Differing from conventional CT scanners, photon-counting detectors convert individual x-ray photons directly to an electric signal, obtaining more detailed information about the interaction between X-rays and the materials they pass through,” Farhadi explains.
“The fundamentally different detection mechanism of PCCT detectors have the potential to overcome limitations of CT detectors—providing CT data at high spatial resolution, with reduced electronic noise, and with inherent spectral information that has demonstrated benefits for various clinical applications.”
For patients, photon-counting scanners are more dose efficient than conventional CT scanners, further reducing radiation dose and use of contrast agent. And physicians benefit from images that have better contrast resolution and visualize very fine tissue structures.
Farhadi was lead author of a paper detailing the mechanics of these detectors and clinical application of the scanner in imaging of thorax in the Journal of Thoracic Imaging 36.2 (2021): 84-94. His illustration of the process was featured on the journal’s cover.
When the PCCT scanner received FDA approval in 2021 after a successful clinical trial, it was recognized by the FDA as “the first major new technology for computed tomography imaging in nearly a decade.”
Based on what they learned from the clinical trial, Farhadi and Saboury turned their attention to a project investigating how PET/CT scanners perform attenuation correction. Attenuation correction involves using CT data to account for variations in tissue density. This correction ensures an accurate measurement of how the radiotracer is distributed within the human body. Farhadi and Saboury thought that utilizing photon counting detectors could enhance this attenuation correction process, leading to a more precise estimation of radiotracer distribution. This enhancement would be particularly valuable in applications such as assessing the metabolic activity of tumors.
“Using spectral information from photon-counting technology we can generate quantitative attenuation maps. These maps would closely mirror the way photons are attenuated in PET imaging, resulting in a more precise calculation of radiotracer distribution,” Farhadi says.
They brainstormed with Sahbaee to discuss the technical details and further expand the concept to various spectral CT techniques. Using a PET scanner with outdated technology that used Germanium to rotate the object being scanned for the correction process, the group began collecting attenuation measurements from a series of scans, as the ground truth. During this process they also came up with an initial sketch of the flowchart of the application.
The three inventors were granted a patent for the new technology in July 2022.
While attending Geisel, Farhadi continues his research at NIH and as director of the Saboury Lab where he leads investigations into applications of advanced imaging techniques in radiology and nuclear medicine. His primary research focus is AI-assisted image analysis of diagnostic and therapeutic radiopharmaceuticals.
“Applying what I learned from research to the clinical experience, and vice versa, is beneficial to both my work at NIH and as a medical student,” Farhadi says. “Also, attending conferences and professional society meetings during medical school gives me a strong foundation for shaping my residency interests.”
Farhadi is applying to dual-board residency programs in nuclear medicine and radiology.