A neuro-oncology research team at Dartmouth’s Norris Cotton Cancer Center, led by the Director Mark A. Israel, MD with first author Gilbert J. Rahme, PhD, recently identified the transcription factor Id4 as a suppressor of tumor cell invasion in glioblastoma. Their paper, “Id4 suppresses MMP2-mediated invasion of glioblastoma-derived cells by direct inactivation of Twist1 function,” was recently published in Oncogene. A key finding was the mechanism by which Id4 silences matrix metalloproteinase 2 (MMP2), determined to be inhibition of the protein Twist1 that is required for MMP2 expression.
“This finding suggests a novel therapeutic target to decrease invasion of tumor cells in patients and may also provide a novel biomarker that could help predict survival of patients with glioblastoma,” explained Israel.
Glioblastoma is the most lethal form of primary brain tumor and leads to death in patients by invading the brain tissue in a process that allows single cells to move through normal brain tissue, which makes complete surgical removal of the tumor impossible. Israel and his team sought to understand the mechanisms that drive tumor invasion of normal tissue in glioblastoma.
Using data from The Cancer Genome Atlas (TCGA), the Dartmouth team demonstrated that Id4 expression correlates with survival of glioblastoma patients and inversely correlates with MMP2 expression. The data suggests that the upregulation of MMP2 resulting from decreased Id4 expression in glioblastoma multiforme (GBM) may contribute to the morbidity and mortality of GBM patients.
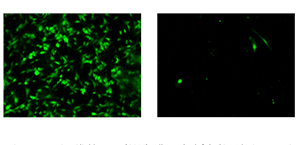
This study used Dartmouth’s Shared Resources including Microscopy and Molecular Biology. “Using the core facilities greatly facilitated the conduct of the work saving time and reducing cost,” Rahme said. All 14 of Dartmouth’s Shared Resources are available to outside investigators by arrangement.
“Conventional drugs targeting the enzymes encoded by MMP genes have not been successful in the clinic due to adverse side effects,” said Rahme. “We believe that proteins in the pathway that controls the expression of MMP2 are likely to be better therapeutic targets. Targeting Twist1 might silence MMP2 and decrease tumor invasion, which will help patients with GBM. Furthermore, the expression of Id4 may serve as a tumor biomarker that can predict the degree of tumor infiltration.”
Looking forward, the therapeutic targets revealed in this study to be actors in tumor invasion need to be further characterized as drug targets and, if possible, therapeutically inhibited. Their pursuit of Id4 as a biomarker for patients with GBM continues in hopes of making useful predictions of tumor invasion and survival.
Israel is the Preston T. and Virginia R. Kelsey Distinguished Chair in Cancer and Professor of Pediatrics and of Genetics at Dartmouth’s Geisel School of Medicine. He is the Director of Norris Cotton Cancer Center at Geisel and the Dartmouth-Hitchcock Medical Center. Rahme is a graduate student in the Genetics Department at Geisel.
This study was supported by a Hitchcock foundation grant for Rahme. Israel’s work was supported by the Jordan and Kyra Memorial Foundation, and the Theodora B. Betz Foundation.
About Dartmouth-Hitchcock Norris Cotton Cancer Center
Norris Cotton Cancer Center combines advanced cancer research at Dartmouth and the Geisel School of Medicine with patient-centered cancer care provided at Dartmouth-Hitchcock Medical Center in Lebanon, NH, at Dartmouth-Hitchcock regional locations in Manchester, Nashua, and Keene, NH, and St. Johnsbury, VT, and at 12 partner hospitals throughout New Hampshire and Vermont. It is one of 41 centers nationwide to earn the National Cancer Institute’s “Comprehensive Cancer Center” designation. Learn more about Norris Cotton Cancer Center research, programs, and clinical trials online at cancer.dartmouth.edu.