
For Release: March 16, 2011
Contact:
David Corriveau 603-653-1978 david.a.corriveau@hitchcock.org
Follow on Twitter: @DartMedNews
DHMC Bariatric Program Earns Top Accreditation Status
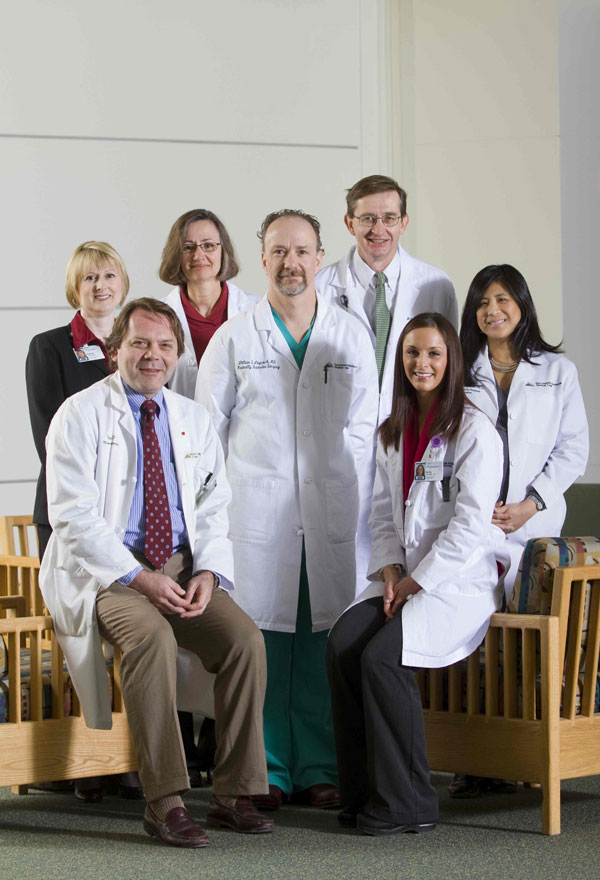
From left to right: Valerie Rescsanski, Administrative Program Coordinator, Thadeus L. Trus, MD, Surgeon, Maureen Quigley, ARNP, Clinical Program Director, William S. Laycock, MD, Program Medical Director, Kelly Barnaby, MS, RD, LD, Clinical Dietician, Paul H. Kispert, MD, Surgeon, Gina L. Adrales, MD, Surgeon
Lebanon, NH—The Bariatric Surgery Program at Dartmouth-Hitchcock Medical Center (DHMC) has earned Level-1 accreditation from the American College of Surgeons Bariatric Surgery Center Network Accreditation Program (ACS BSCN).
This milestone recognizes the skills and experience of DHMC's surgeons and support staff who deal with a high volume of patients undergoing weight-loss surgery, as well as an institutional commitment to maintaining outstanding facilities, safe high-quality care, and monitoring patient outcomes.
"We've been working toward this for a number of years," says William S. Laycock, MD, director of the bariatric-surgery program and an associate professor of surgery at Dartmouth Medical School. "This is a great reflection of the hard work of all those involved with the program.
Bariatric surgery is performed on morbidly obese people who have failed to lose weight through conservative management, and who meet guidelines established by the National Institutes of Health (NIH). DHMC established its program in 1972, and now comprises four surgeons, a nurse practitioner, two dieticians, and other support staff. It is the longest continually operating bariatric surgery program in northern New England, and one of three Level-1 programs in the region.
At DHMC, most patients undergo bariatric surgery via the laparoscopic method, with small incisions, which generally result in a shorter recovery time. Other procedures include:
- Gastric bypass, which reduces the size of the stomach and reroutes a small portion of the small intestine so that the patient feels full after eating a small amount of food and absorbs fewer calories. It is considered the "Gold Standard" of bariatric surgery and has been well-studied, producing the best long term results.
- Laparoscopic adjustable gastric banding, which reduces the size of the stomach with an adjustable silicone band. Periodic band adjustments are needed.
- Laparoscopic sleeve gastrectomy, which reduces the size of the stomach by removing a portion of the organ.
- Bariatric revision, which clinicians perform to correct a complication from a previously performed, outdated procedure, such as a vertical-banded gastroplasty.
About one year after bariatric surgery, patients usually lose between 30 and 70 percent of their excess body weight, depending on the procedure and patient compliance. Patients must follow a healthy diet and exercise regularly for life to keep off the weight. According to a landmark study published in the Journal of the American Medical Association in 2004, following bariatric surgery:
- Type 2 diabetes went into remission in 76.8 percent of patients, and 86 percent experienced significant improvement
- Hypertension was eliminated in 61.7 percent of patients, and significantly improved in 78.5 percent
- High cholesterol was reduced in more than 70 percent of patients
- Sleep apnea was eliminated for 85.7 percent of patients
- Joint disease, asthma and infertility were also dramatically improved or resolved.
Two additional surveys published in the New England Journal of Medicine suggest that bariatric surgery may extend the lives of morbidly obese individuals by 30 to 40 percent.
The ACS network of bariatric surgery programs accredits facilities in the United States through "independent, voluntary, and rigorous peer evaluation in accordance with nationally recognized bariatric surgical standards," according to the network Web site. "With the expanded range of facilities now engaged in bariatric surgery - from full-service inpatient hospitals to outpatient facilities - ACS BSCN accreditation symbolizes institutional commitment and accountability for safe, high-quality surgical care."
Hospitals earn Level-1 accreditation by demonstrating the capacity to manage and commit resources to complete bariatric surgical care. They must engage patients at all levels of obesity and set standards of care for weight-loss operations, ages, co-morbid conditions, and re-operations. Level-1 facilities must perform 125 or more weight-loss operations a year, with one credentialed and experienced bariatric surgeon who has performed at least 100 weight-loss operations in the previous 24 months. All centers with ACS BSCN accreditation also must collect extensive data on all cases, which ACS keeps in a central proprietary database accessible to participating centers for quality measurement and improvement purposes.
"The need for these services continues to grow," Laycock says. "An estimated 22 percent of adults in New Hampshire qualify for these forms of surgery. It's very much an under-utilized resource."
-DMS-