Geisel MD Curriculum
Geisel’s integrated four-year medical curriculum provides a strong foundation in the basic sciences, offers exceptional clinical experiences, and emphasizes inter-professional collaboration and teamwork. We are committed to innovation and quality improvement, and continually refresh our curriculum to prepare students to address contemporary issues in healthcare and keep pace with medicine’s rapid advances. Our students develop competencies in eight broad areas: medical science; clinical care; population health; communications skills; personal, professional and leadership development; evaluation and improvement in medicine; professionalism; and collaboration and teamwork. Dartmouth’s small class size provides an intimate learning community where students develop close relationships with faculty and colleagues that foster collaboration, inquiry and engagement.
Our curriculum comprises three phases of learning: Foundations of Medicine, Clinical Immersion, and Exploration and Differentiation.
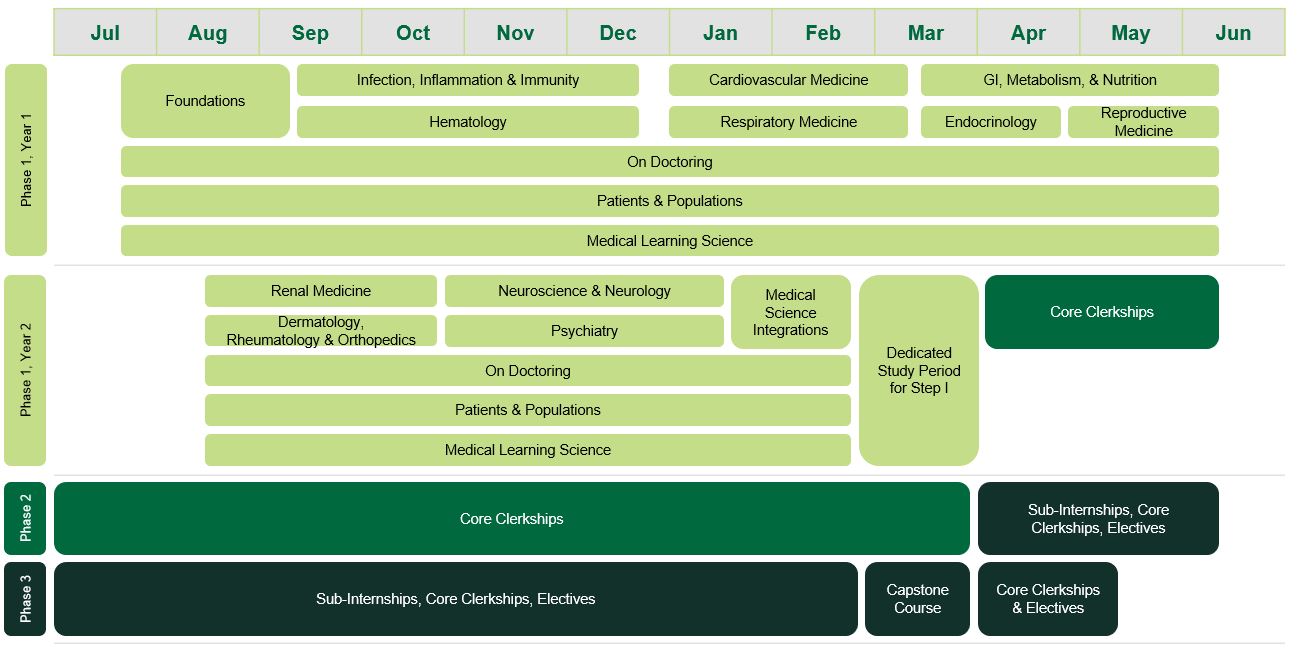
Phase 1: Foundations of Medicine
Phase 1 consists of courses organized into blocks and longitudinal courses that span the entire year. All courses are highly integrated and contain longitudinal curricular topics and curricular threads. An 8-week summer break between blocks 4 and 5 provides students with the opportunity to pursue research, quality improvement, clinical experiences, or other personal interests.
Block 1 – Foundations of Biomedical Sciences
Block 2 – Infection, Inflammation & Immunity; Hematology
Block 3 – Cardiovascular Medicine; Respiratory Medicine
Block 4 – GI, Metabolism & Nutrition; Endocrinology; Reproductive Medicine
Block 5 – Renal Medicine; Dermatology, Rheumatology & Orthopedics
Block 6 – Neuroscience & Neurology; Psychiatry
Block 7 – Medical Science Integrations
| Longitudinal Courses | Longitudinal Curriculum | Longitudinal Curriculum |
Phase 2: Clinical Immersion
This phase begins in April of the second academic year. It includes required clerkships in seven major clinical disciplines: Internal Medicine, Surgery, Obstetrics and Gynecology, Pediatrics, Psychiatry, Neurology, and Family Medicine. These clerkships are four to six weeks in length and are completed at a variety of settings including our two affiliated academic medical centers (Dartmouth-Hitchcock Medical Center and the Veterans Affairs Medical Center in White River Junction, Vermont), regional teaching hospitals, regional office practices, and more distant medical centers and hospitals to provide our students with an exceptionally broad array of clinical clerkship experiences. Geisel-affiliated clerkship sites include Indian Health Service medical centers in Arizona and New Mexico; Hartford Hospital in Connecticut; Santa Clara Valley Medical Center, California Pacific Medical Center, and Children’s Hospital of Orange County, in California. The Clinical Immersion Phase allows ample time to explore specialties and electives with a schedule that allows students to take up to eight weeks of clinical electives along with the seven required clerkships.
Phase 3: Exploration and Differentiation
Starting in April of the third academic year, this phase includes one required four-week clerkship (Advanced Ambulatory Medicine) and at least one advanced four-week sub-internship in one’s field of choice. By completing required clerkships by April of the third academic year, Geisel students have 5-6 months to explore career choices through electives and sub-internships prior to needing to apply to residencies. Students may choose from a wealth of opportunities on campus, across the US, and around the world. Students can also design their own elective with the support of a Geisel faculty member. In the latter half of the fourth academic year, all students return to campus for a capstone course that focuses on knowledge and skills important in residency, including advanced clinical skills, application of foundational medical sciences to clinical care, and quality improvement. These topics prepare students to excel during their residency programs and enhance lifelong learning skills.