By,
India Burdon Dasbach MED’25
Participating in the James Strickler Clinical Elective in Global Health exchange program in Dar es Salaam, Tanzania, was the highlight of my time as a medical student. Before traveling to Tanzania, I had the pleasure of working with the Muhimbili University of Health and Allied Sciences (MUHAS) medical exchange students from Tanzania, David Muhunzi and Stella Kaihula, who spent nearly two months on clinical rotations at Dartmouth Health last fall. While I was sad that our time at Dartmouth ended, I stayed in contact with them via WhatsApp, as they helped prepare me for my time at MUHAS this past January.
I spent two months in clinical rotations at Muhimbili National Hospital, rotating through General Surgery, Emergency Medicine, Obstetrics and Gynecology, and Infectious Diseases. I participated in caring for those with a wide range of diseases and gained a thorough understanding of how healthcare provision works at the largest tertiary hospital in Tanzania.
In General Surgery, I rounded and assisted in lab draws and helped with patient care on the wards and during surgeries. In the “operating theatre,” I saw a wide range of surgical procedures, all of which were done in an open rather than laparoscopic technique that is more common in the U.S. Some examples include surgeries to remove tumors in the small and large intestines, removal of the gallbladder, removal of breast lumps and cancers and many more. I also observed skin grafts for burn surgeries with plastic surgeons, tumors removed from the brain with neurosurgeons, and tumors removed from the head and neck with ENT surgeons.
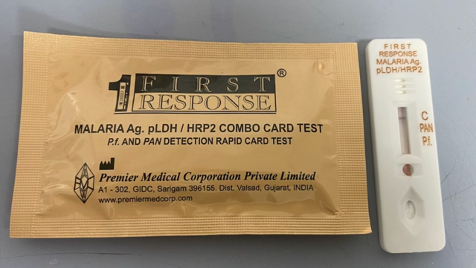
Next, I rotated in the Emergency Department (ED) for two weeks and saw a great variety of cases. In the adult ED, I saw acute presentations of HIV, TB, and malaria, in addition to undifferentiated sepsis, kidney failure, liver failure, trauma from motorcycle crashes, burns from stoves, and several electrocution burns. In the pediatric ED, I saw new presentations of cancer, aplastic anemia, gastroenteritis, burns from stoves/cooking oil, nephrotic syndrome, malnutrition, heart failure in children with congenital heart disease, pyloric stenosis in a young baby, and malaria.
I assisted other medical students with IVs and blood draws, pushed medicines handed to me by the nurses, and helped with traumas and various minor procedures. There were a couple of cases I could take a history with, in English, but for the most part, they spoke Swahili, so I teamed up with a medical student who would translate, and then we would go over the differential diagnoses and plan together. Residents were happy to teach me throughout each case, ask me about differential diagnoses and plans, and have me read EKGs and point out what I noticed on images for my practice.
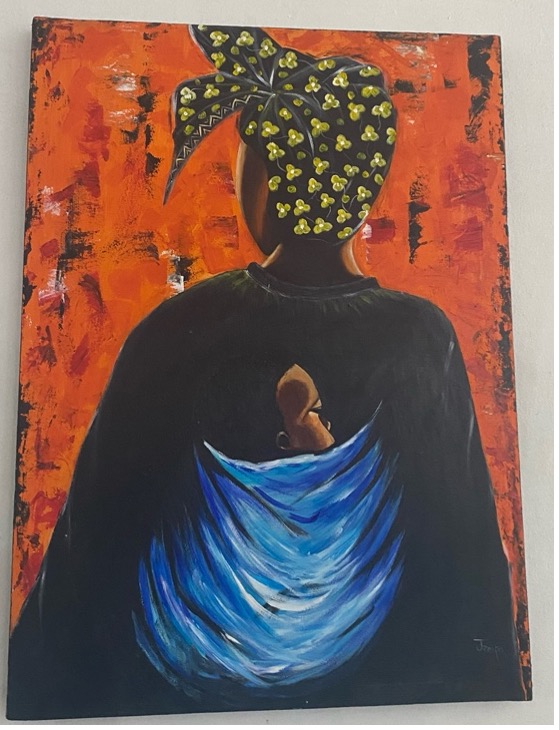
Third, I rotated through Obstetrics and Gynecology (OB/GYN). The department comprises high-risk obstetrics, including a dedicated maternal ICU, normal-risk obstetrics, oncology, and gynecology, plus a dedicated OB/GYN “operating theatre” and outpatient clinics. In the obstetric wards, I saw many sick women, including mothers in the ICU with kidney failure requiring dialysis after severe pre-eclampsia. I saw a mother with postpartum cardiomyopathy in heart failure, a mother with end-stage cirrhosis with stillbirth, and a mother with sickle cell experiencing acute chest syndrome post-delivery. I observed the resuscitation of one neonate, who was then successfully stabilized on CPAP (continuous positive airway pressure) in the neonatal ICU. I also observed the birth of a baby with anencephaly, a condition I had never seen before. In labor and delivery, I observed vaginal deliveries and noted that epidurals were not available for mothers, so births were done without pain medication.
In GYN, there was a very high prevalence of cervical cancer. I had the opportunity to go on a field trip with the other medical students to the Ocean Road Cancer Institute, where most received cancer care and chemotherapy, visited radiation facilities, and learned from Tanzanian cancer care experts. In the theatre, I observed many cesarean sections, including for twins and triplets. I also observed open surgeries to remove tumors and cysts of the female reproductive organs, and hysterectomies. In the outpatient clinic, I was a part of antenatal care visits, family planning, and a special clinic for mothers with sickle cell disease who often experience pregnancy loss.
Finally, I rotated in Infectious Diseases (ID), where I saw a breadth of diseases endemic to Tanzania that are not as common in the United States. With the ID team, I helped care for those with both pulmonary and extrapulmonary tuberculosis (TB), severe malaria, and infected wounds - as well as HIV with AIDS-defining illnesses, including cryptococcal meningitis, toxoplasmosis, pneumocystis jirovecii, and even a case of measles. The ID team was sure to ask students many questions on rounds and assign topics to read about and present on rounds the next day.
Throughout my experience at MUHAS, I was mentored and guided by Dr. Maryam Amour, a physician-scientist and lead TB researcher. Dr. Amour gave visiting exchange students a tour of the Infectious Disease Institute. I also met with Dr. Albert Magohe, who works closely with the DarDar HIV program and runs the new hyperbaric chamber in Muhimbili. I was also fortunate to meet Professor Patricia Munseri, a leading physician-researcher in infectious disease, at her office for the HIV vaccine trials. I assisted her research in developing a RedCap Database for surveys of female sex workers taking PrEP.
In my free time, I took an introductory Kiswahili course twice a week for eight weeks, explored the many wonderful restaurants in Dar, visited Zanzibar and Mafia islands, experienced the busy Kariakoo market, learned to cook ugali and pilau from my Tanzanian friends, and much more! I had an incredibly impactful experience in Dar es Salaam that truly enriched my medical education. I was so welcomed by staff, students, and physicians at MUHAS and Muhimbili, and felt warmly welcomed by the people of Dar es Salaam, who often greeted me with a smile and “Karibu Tanzania” or welcome to Tanzania on the streets. I achieved my academic goals of understanding healthcare provision in a resource-limited setting in the inpatient wards, operating theatre, and ED while gaining experience and exposure to diseases that are less common in the United States and understanding the medical education system in Tanzania.
I am so grateful and proud to have been sponsored by Geisel’s Center for Global Health Equity - which supports equitable bilateral exchanges in global health through its long-standing relationship with MUHAS and Muhimbili National Hospital. I also would like to thank Dr. Donald MacDonald MED’80, for providing funds to the Center for Global Health Equity to make the experience possible. Dr. MacDonald is an American Ophthalmologist who has engaged extensively in global health work during his career, notably in Ghana and other countries in Africa. In 2016, he established an endowed fund in the Center to support global health experiential learning for Dartmouth’s medical students at our partner institutions, including MUHAS.
Given the historical backdrop of colonialism, neocolonialism, exploitation, and white saviorism in global health work, I am still developing how I will incorporate my interest in global health in my career as a physician in an ethical, equitable, and sustainable fashion. The James Strickler Clinical Elective in Global Health has given me the experiences, connections, and growth mindset to embark on this journey. I could not be more excited to use my experience as a launching point for future global health collaboration, scholarship, and education.