Dear friends and colleagues,
As many of you know, our beloved colleague Eugene (“Gene”) Nelson, DSc, MPH, transitions to emeritus professor of health policy and clinical practice and community and family medicine at the end of June, after more than 40 years at Dartmouth. Gene is a national leader in health care improvement and the development and application of measures of quality, system performance, health outcomes, value, and patient perceptions. He is the recipient of The Joint Commission’s Ernest A. Codman award for his work on outcomes measurement in health care. Gene has been a pioneer in bringing modern quality improvement thinking into the mainstream of health care; he helped launch the Institute for Healthcare Improvement and served as a founding board member.
Gene received an AB from Dartmouth College, an MPH from Yale University, and a DSc from Harvard University. He joined the Dartmouth Medical School faculty as assistant professor of community and family medicine in 1978. His earliest published work focused on the emerging role of physician assistants. He was one of the first health services researchers to explore the influence of patient perceptions on treatment adherence and outcomes and patient-reported functional outcomes, fields that would blossom over the next four decades and emerge as the scientific underpinnings of the biopsychosocial model, a countervailing force to the biomedical model that upheld the primacy of anatomic and physiologic outcomes at the time.
A review of Gene’s CV is like a walk through the halls of history of health services research and a testimony to his profound impact on our field. In 1984 alone he published both a curriculum to increase physicians’ consciousness of cost and a trial to improve older adults self-management skills, laying the earliest foundation of what would become a coproduction learning health system.
In 1986, Gene was recruited by Paul Batalden, emeritus professor of health policy and clinical practice, pediatrics, and community and family medicine, to work for the Hospital Corporation of American in Nashville, TN. During this time, Gene continued to publish as a team member of one of the most influential population-based studies in our field, the Medical Outcomes Study. This two-year study of more than twenty thousand persons with chronic health conditions ushered in the modern era of patient-reported outcomes measurement with the introduction of the SF-12, SF-20 and SF-36 measures of quality of life, as well as measures of patient adherence, mental health, sleep, sexual function, and social support. Elliott Fisher, professor of health policy and clinical practice, medicine, and community and family medicine and former Director of The Dartmouth Institute (TDI) observed, “Gene Nelson has had an extraordinary impact on the fields of health services research and quality improvement. There was a time when clinicians did not believe that patients should be trusted to judge their functional status. Through his work on the Dartmouth COOP Functional Assessment Charts (1980s) and then as a leader in the Medical Outcomes Study (1990s), Gene helped catalyze a revolution: we must and can measure what matters to patients—how they evaluate their functional status and quality of life. The instruments he helped develop are still in wide use throughout the world.”
Gene returned to Dartmouth in 1992 as the Director of Quality Education, Measurement and Research at the Dartmouth Hitchcock Clinic (now DH) as a professor of community and family medicine. At that time, he and colleagues began developing clinical microsystem thinking. His work developing the clinical value compass and whole system measures to assess health care system performance has made him a well-recognized quality and value measurement expert. Fisher shared: “Many believed—and too many still do—that the way to improve care was to tell people to do a better job. Gene was a leader in debunking that idea and instead giving clinical teams and health care leaders the knowledge and skills needed to actually improve. He helped launch and was a founding board member of the Institute for Healthcare Improvement, which now supports improvement in health and care across the globe, reaching tens of millions of people each year.”
Batalden remarked on Gene’s “deep curiosity about the real world of health and healthcare service…and the way it all works—especially the way users see it. When there was interest in getting systematic user feedback from physicians, nurses and patients about the experience of using a hospital, Gene created a family of survey research measures based on the hospital experience that was grounded in a shared understanding of the core hospital processes. When the interest in teaching quality improvement in professional education settings emerged, teachers struggled to get the content correct and Gene suggested the creation of a week-long summer camp for teachers of nurses, physicians and administrators. When the proliferation of outcome measures dramatically expanded, Gene created the value compass—to create a set of simple categories for balanced measures of outcomes. When there was interest in opening a deeper exploration of the “front-line work” of a clinic or a hospital, Gene worked with Brian Quinn and others to create a course on the clinical microsystems of healthcare service.”
In 2014 Gene “retired” from DH and became a primary faculty member at TDI. During the last decade, he integrated the two major themes of his lifelong work—recognizing patients as experts in their own health and empowering clinicians with the tools they need to improve care delivery—by establishing patient-centered registries and developing learning health systems capable of coproducing improved health care and innovative science. He led national proof of concept demonstration programs for several populations including persons with cystic fibrosis, inflammatory bowel disease, and rheumatology, and those receiving palliative care services. Under his leadership, this work has been implemented at Dartmouth Health as the Promise Partnership. Fisher lauded the Promise Partnership as a “model for health care transformation, which brings these two threads of his career together by putting in place a learning health system where real-time measures of clinical, patient-reported and clinical team member experiences are used to support continuous improvement in health, care and science.” Gene handed off Promise Partnership leadership to Anna Tosteson, James J. Carroll Professor of medicine and health policy and clinical practice and former interim director of TDI, Brant Oliver, associate professor of community and family medicine, psychiatry, and health policy and clinical practice and system Vice President for Care Experience for the Dartmouth Health system, Megan Holthoff, Research Project Director, and Aricca Van Citters, Senior Research Scientist. Tosteson noted, “Gene was a key instigator and champion for the Promise Partnership learning health system and masterfully guided our pilot efforts in oncology and beyond. We are fortunate to be able to build on this both through the Dartmouth E-STaR Center and SYNERGY.”

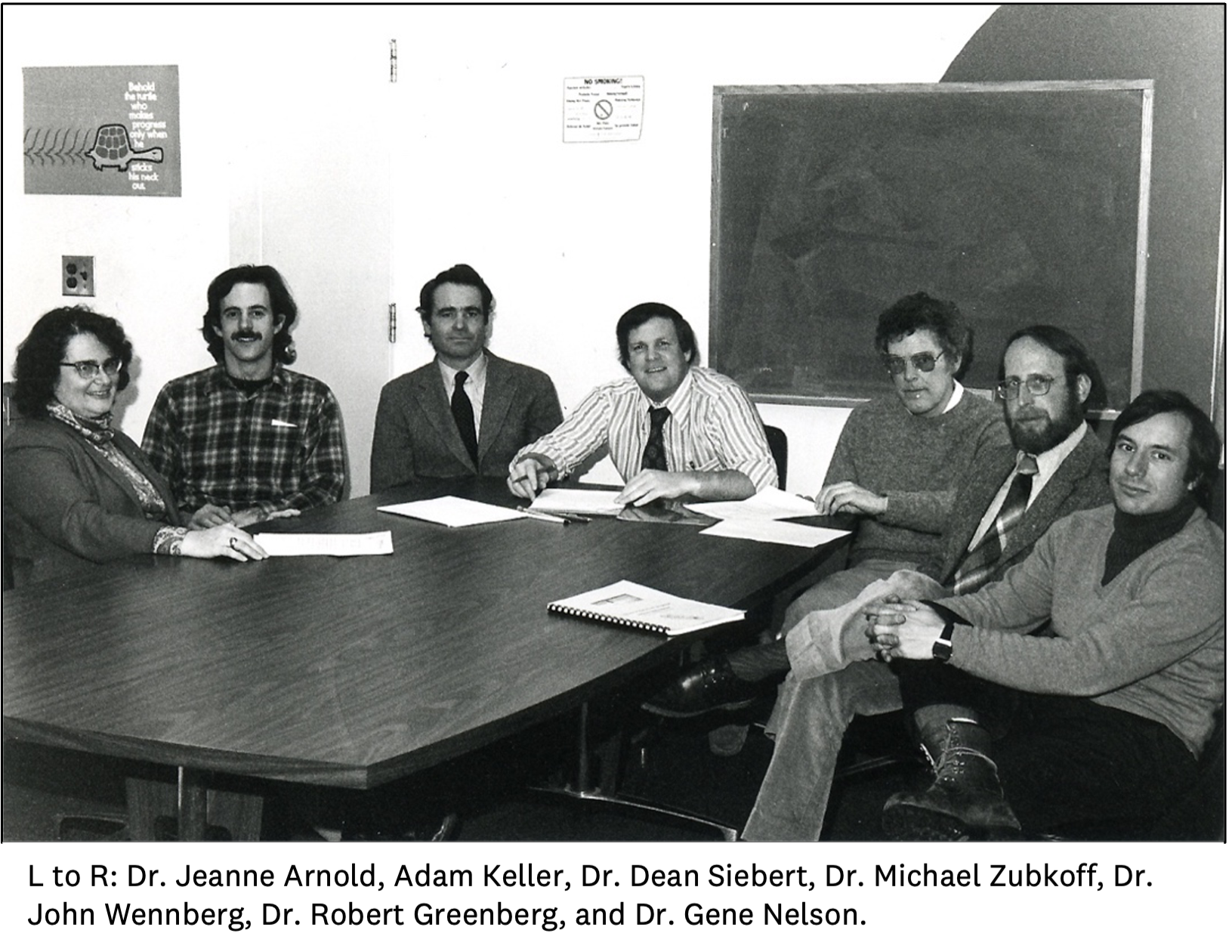
Mike Zubkoff, professor of community and family medicine and health policy and clinical practice, was not surprised to learn that Gene was trying to “slip off without a special occasion.” (Gene capitulated to a picnic earlier this month with CoProduction Lab team members and three begrudgingly invited TDI Directors, above). Zubkoff continued, “As one of our world’s leaders in health care improvement and the development and application of measures of quality, system performance, health outcomes, value, and patient and customer perceptions, Gene has been my inspiration, mentor, colleague, and close friend for nearly 50 years! Gene is the most visionary, effective, and humble colleague with which I have had the honor of working.” Batalden, summing up Gene’s genius, explained, “He recognized that social science development and application was rarely a soloist’s enterprise. He attracted the curiosity and energy of many others. He knew what encouragement meant for someone trying to learn or write or analyze data. He listened carefully, so he was always fun to talk to. In short, he modelled what it meant to have joy in work and learning.”
We all know that Gene doesn’t like to be the center of attention, and that is perhaps one of his superpowers. Indeed, Gene’s main advice to me when preparing this announcement was “Less is more.” Gene has made a career of collaboration and of putting others first – patients, hardworking providers, and his many healthcare improvement colleagues. Gene will be deeply missed, and we are grateful for his legacy. Zubkoff captured these sentiments perfectly, “Gene’s career accomplishments have truly improved health care around the world!”
Megan Holtoff asks “If you have had the privilege of interacting with Gene over the years or have witnessed moments where his passion and dedication inspired those around him, we kindly ask you to share any stories you may have. Whether it's a meeting where Gene delivered an inspiring presentation, a research collaboration that left a lasting impact, or simply a candid moment where his enthusiasm for his work shone through, we would be grateful for your contributions. Potential ideas may include:
- I’ve always wanted to tell Gene…
- When I think of _____, I think of Gene.
- Gene is best at….
Please contribute any stories you wish to share by June 30th using the following link: https://ellacard.com/sign/f8076742-ac33-4318-922f-0ede0afb1233. Your stories will serve as a true testament to Gene's legacy.”
Join me in thanking Gene for this legacy and for continuing to inspire all of us to make health and healthcare better for all.
- Amber Barnato, MD, MPH, MS
John E. Wennberg Distinguished Professor
Department Chair and Director of The Dartmouth Institute for Health Policy and Clinical Practice